|
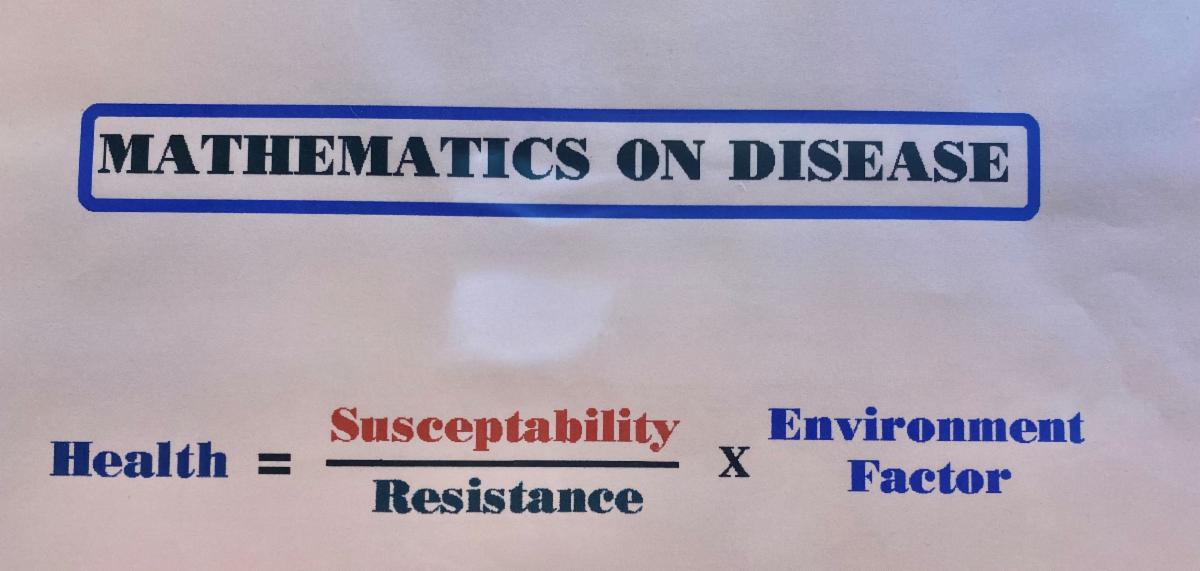
Another week goes by, as we seem to settle into this COVID-19 pandemic. Like 9/11 things may never be the same once this has passed. Who would have ever thought you would have to take off your shoes and be scanned before boarding an aircraft before 2001? Or carry on a bottle of water? We will get through COVID-19, but it will be a little different when we reach the other side and find the new normal. Perhaps we will make lemonade from lemons and be better off for the next time. “AIDS will be resolved one day, I’m confident of this, but society will always face epidemics to replace it.” We have always had epidemics. Whether it be Tuberculosis, Syphilis, SARS, Leprosy, Cholera, and the list goes on. What we don’t know is what group or groups will be affected next. With AIDS/HIV in the 1980s, it was the LGBTQ community. COVID-19 may have more serious consequences for the African American population. It’s a moving target! Staying home this weekend, I had some time on my hands. I came across some old files hidden away. I found some slides I made from the 1980’s. Back then, I made my own slides using my 35mm camera. I would take pictures of the information that I typed on a piece of paper and then took the film to the drug store to get it processed into slides. Wow, how things have changed! I came across a slide I made years ago titled “Mathematics of Disease”. I do believe this equation is timeless, and certainly holds true today. Let me explain the picture above detailing this equation: Health (or lack of) = Susceptibility (the numerator) -- The likelihood or liability to be influenced or harmed by a particular thing. Susceptibility increases when people don’t take care of themselves: medical problems not optimally controlled, no exercise, eating poorly, smoking, poor sleep, lack of barriers or increased exposure to pathogens, stress, and so on. Each factor synergistically increases susceptibility to disease. ÷ Resistance = The ability to not be affected by something, especially adversely. Resistance is increased with vaccinations, exercise, eating nutritiously, positive mental attitude, getting enough sleep, and general measures to stay healthy. Resistance is reduced with a compromised immune system, co-infections, malignancies, poor health, general inflammation, sleep deprivation, and stress. x Environmental Factors = Any factor (living or non-living) that influences living organisms. Prevalence of a germ (COVID-19) in the population is certainly the first environmental factor that comes to mind. Other factors include overcrowding, the air we breathe, aging, water pollution, cleanliness, co-existing diseases, and environmental stress to name a few. It’s not one particular item in this equation that defines health or lack of it, but many. You should do what you can do for each part of the equation to assist yourself in staying well. Wear facial coverings. Keep your distance when around others. Wash your hands often. Stay active. Do some deep breathing. Eat better. Reduce your stress loads in ways you can. Each and every positive action you take to increase your resistance will shift the equation in your favor. Each and every action you take to decrease your susceptibility will help keep you healthy. COVID-19 testing is great; however, you can test negative on a Monday and turn positive on Tuesday. This test is useful for diagnosing current COVID-19, but not useful in predicting future infections.
When the antibody is approved, after demonstrating the right specificity and sensitivity of the test, that may be useful to reduce susceptibility and environmental factors by knowing who is immune and who isn’t. There is no one test or action a person can take to totally eliminate risk. This is true for everything we do from taking a walk to sky diving. It’s a balancing act with decisions made by each individual, hopefully with a good data base for guidance, in making the best decision for yourself. We used to call it “Universal Precautions.” That’s what the medical professional would do by treating every person the same way regardless of knowing if they had a communicable disease or not. The provider would protect themselves as if everyone they came in contact with was infectious. The practice of universal precautions still applies. That’s what risk reduction is about. Whether it be HIV, STD’s, colds, coughs, staph infections, or anything else, appropriate preventive protections should be put in place all the time. It’s your responsibility to be knowledgeable. The mathematics of disease will change as information evolves and this is occurring at a rapid pace. What we think is true today may not be true tomorrow. Vaccines will maximize resistance. Hopefully an effective one for the COVID-19 virus will be available as soon as possible. Vaccines reduce susceptibility and environmental factors by increasing resistance. None of these measures, by itself, will be the solution; however, a combination of them most likely will. As for the Be Well Medical Center, I’m proud to work with a group of medical heroes. We come to work everyday with kindness, gentility, patience, compassion, and smiles. My staff puts themselves at risk everyday and are helping the lives of our patients. Evening clinics are still suspended although we are extending back our daytime clinic hours to 5 P.M. beginning Monday, April 27. Patients are being screened at the front door for COVID-19 symptoms and temperature. We appreciate everyone arriving with their own facial covers. We wish you well, and are here for you during these difficult times! To Your Good Health…We Remain!
13 Comments
We hope this email finds you well. We appreciate all the great feedback we’ve received regarding our weekly email outreach to you during this pandemic. We thank each of you who have shared words of encouragement to us.
We are here for you and again seeing patients in the office. We are also back to accepting new patients. We continue to do “drive-by” COVID testing for our patients only. We are treating those who are mild to moderately infected and referring to our specialists those requiring more intensive care. Those patients potentially infectious will be screened by a health care provider before entering the office. If you do come to our office, we request you bring a facial cover and maintain a 6-feet distance from others whenever possible. Everyone entering the building, including our staff, will have their temperature taken at the front door. We are managing more cases of COVID-19 than we could ever have expected. Our team of health care providers are doing a superb job of reaching out to our COVID-19 infected patients daily on the telephone to see how they are doing. I believe we have truly kept many of our patients out of the hospital; who may have ended up there, if not for our dedicated and aggressive approach. Additionally, Med-Shop pharmacy in the building has worked hard to find hydroxychloroquine (Plaquenil) and Zithromax to treat our patients when necessary. This COVID-19 scenario reminds me of the 1980’s when many physicians refused or did not want to treat AIDS patients, just like COVID-19 now, for a variety of reasons (some not so good). We have always offered compassionate care to those living with HIV and that decision made me become a better person and primary care physician. Our team is committed to manage your care through the COVID-19 crisis. We continue to perform COVID-19 nasal swabs and usually get results in 1-3 days, depending on their backlog. I’m still being the “squeaky wheel” with Abbott Diagnostics to get the rapid 15-minute test kits in our office. When we get them, we will be able to give results in minutes instead of days. They will not release them to us yet, but we are not giving up hope to get them soon. It’s frustrating that we are one of the few primary care offices with the correct equipment to run these tests; but can’t get the test kits. I will not stop trying to get them as quickly as I can. I even offered to loan my equipment to a center that is testing to help them out. It’s shameful my testing platform sits idle. I would like to explain testing for COVID-19 as it can be confusing, especially when the antibody test is expected to be released shortly. The current nasal swab test detects whether the COVID-19 virus is present in your body or not. A positive test means the virus is present in your body. A negative test means that no COVID-19 virus was found. This test can also be referred to as a Polymerase Chain Reaction (PCR) test. The antibody test should be approved by the FDA soon. Currently this antibody test is not approved for use. I’ve heard of one urgent care center doing them for $50.00 as a “drive-by”. I don’t understand how this can be and at this time I personally don’t trust it. I heard Beaumont Hospital is doing a clinical trial on the antibody test, but have no other information on that at this time. If the antibody test is positive, that means the person has had the COVID virus. The antibody test does not indicate whether or not the person currently has the virus. The two tests combined, nasal swab (PCR) and blood antibody tests, when used together will be very useful in determining a person’s status regarding COVID. If someone is both COVID-19 antibody positive, and nasal smear (PCR) positive, that would mean they are recently infected and has not yet cleared the virus. These tests are very familiar and similar to HIV testing, treatment, and prevention programs that we have been utilizing with success for years. Now is not the time to practice those five deadliest words “Maybe It Will Go Away”. If you have any health concerns, lets manage them early on. What we need right now, all of us, is to have plenty of compassion, kindness, gentility, patience, and smiles. Do what you can do…eat right, move around and stay active the best you can, check in on friends and family, and keep a good attitude! To Your Good Health…We Remain We hope all of our patients are staying home and sheltering in. We, at Be Well Medical Center, are adjusting to our “new normal” and operating better than we ever could have expected. We’re delivering excellent health care on the computer via telemedicine or telephone for those unable to connect online. The process has gotten much easier and now we can simply send you a text message before your scheduled telemedical visit; and if you reply to that text you will be connected automatically instead of going through our portal system. BY DIRECTIVE OF THE CENTER FOR DISEASE CONTROL, NOW IS NOT THE TIME TO PERSONALLY SEE YOUR DOCTOR UNLESS ABSOLUTELY URGENT. (cdc.gov) We have some telephone lines and medical visits being managed by our staff from their homes to limit exposure to COVID in our office. We are all doing well, especially our employees who had COVID. Most importantly, our care for immediate concerns has not been interrupted and is being handled immediately. In fact, many patients are commenting that it’s faster access to us than ever before. Per CDC guidelines, we are trying not to spend our precious time writing “back to work” notes. The CDC has declared a medical emergency and as such work notes should not be expected. We have extended no foot traffic visits for another week until April 20, 2020. However, don’t delay in reaching out to us as we have been very creative and are able to handle most concerns remotely. We are now accepting new patients again for telemedical visits as our situation has stabilized. Again, requesting your refills through your pharmacist electronically saves us time and gets this done more quickly. We also are able to manage COVID-19 efficiently and keep you out of the Hospital more often than not. We continue to do “drive by testing” for our patients and provide early treatment with Hydroxychloroquine and Zithromax when indicated. Our network of Specialists has been diligent in communicating with us as the need arises and quickly seeing our patients with our referral in the hospital as appropriate. On a somewhat disappointing note, we have not been able to get the 15-minute test kits in the office (yet). We have the correct devices to do the tests, but not the test kits. They are being given to hospitals and nursing homes only. I have added my letter to Abbott Laboratories regarding this concern at the end of this communication for you to read. We will get through this together. CDC guidance recommends everyone going outside for essentials wear any type of cloth over their mouths and noses. This offers some protection to you and those around you. It is a recommendation at this time and not an order. We are here for you. Again, I’m so proud of my entire staff for giving over 100%. Thank you for all the warm thoughts and praises we have been receiving. They mean a lot to us! To Your Good Health…We Remain Copy of My Letter to AbbottApril 6, 2020 Robin Cook Abbott Laboratories Dear Robin, Thank you for taking your precious time and joining me on a telephone call this afternoon. There is a problem to be dealt with regarding distribution of the Rapid COVID-19 kits and it requires immediate attention. I’m not sure how to do it, and request escalation to the correct individuals that can solve it for me; and for other providers like me. As I have made you aware, I have a medical practice in Berkley, three miles north of Detroit. I have been in practice since 1980. I’m a board-certified family doctor, a certified research professional conducting many HIV clinical trials, and an accredited HIV specialist with the American Academy of HIV Medicine. I tell you this because my medical experience is relevant to our current COVID-19 pandemic. I started my practice at the very beginning of the AIDS epidemic. I direct four medical providers and together we manage over 1000 HIV patients. Additionally, we have many other patients that are high risk for COVID progression. I feel like I’m reliving the AIDS crisis all over again without the stigma or prejudice of the LGBTQ population. If doctors such as I don’t ACT-UP, nothing will happen to help assist my population of patients. Just like in the 1980’s my clinic has not shirked away from our duty of taking care of our patients during this pandemic. We have been doing at least 50 telemedical visits daily from sick or worried patients. We do drive-byes for COVID tests of which we currently get the results back in 2-3 days. Six of my medical staff have become infected with COVID, yet most of them are currently working remotely from home. I rotate 2 medical providers working remotely from home and two in the office caring for patient on the telephone or computer. We are closed for foot traffic. We have been able to manage our own patients with immediate service. We are managing well over 40 patients with COVID and the list keeps growing. I am most proud of our response, probably not much different from many other primary care providers, especially those who lived through the early days of HIV. I’m not complaining, but I’ve learned from the past that I have to advocate for my patients. When the times get tough the tough get going and there needs to be change in the distribution of the rapid COVID tests. Abbott has made a blanket “cookie cutter” decision to not provide the test kits to primary care clinics and only to hospitals, including designated hot spots. I understand there are priorities, however there are also exceptions that must be made. “The horse is out of the barn and to do these tests strictly in the hospitals is simply wrong. I want to augment the hospital system and not replace it. I want the opportunity to practice prevention and early detection to help stop the spread and to treat early to prevent hospitalizations, ventilators, and mortality. The problem is this. The 15-minute Abbott platform has just been released to do COVID-19 testing. My clinic is fortunate that we already have the correct lab equipment in place to run these potential lifesaving tests. All we need is the kits to accomplish this, yet I was just told I can’t receive any. Any clinic such as mine should be considered a priority. Patients prefer their own doctor that they are comfortable with and would seek medical attention sooner rather than later to wait in a dreaded line at the hospital. The fact of the matter is I’m seeing plenty of these patients right now. Hospitals are the worst place to be unless they are necessary. We status our patients from mild to severe. We call them daily to update their conditions. I’m already prescribing hydroxychloroquine and Zithromax to the moderate intensity patients and sending to the hospital the severe cases. Providing care at this grass root level is one of the best places for testing for so many reasons. Abbott, or whoever makes the decisions doesn’t seem to get this priority. Rapid COVID testing may not be right for every office, but it is for my clinic. Any request must be individually considered immediately. Lives are at stake. I’m more than willing to be part of the solution. Please respond to me as soon as possible. Respectfully, Paul Benson, D.O. The COVID-19 crisis is surreal. We are already managing more COVID patients than I ever expected to. It was only a few weeks ago that everything appeared so normal. COVID-19 has affected us all in so many different ways (physically, mentally, economically, and more). When we get to the other side of this pandemic, I would like to think the world will be better off and we have learned to be a more compassionate and kinder place. This crisis has made me think back to the similarities from the 1980’s AIDS epidemic. I was a brand-new young doctor at the time. Caring for HIV patients since 1980 has influenced my life in so many ways. It made me a better physician. Perhaps COVID-19 will do the same for others.
We have been serving our patients with telemedical visits and “drive by” COVID-19 testing since the onset. Patient response has been nothing short of amazing. Our patients have been eager to use their smartphones and laptops to connect with us. We are overwhelmed, but handling our situation well mainly because of a set of special health care providers and a dedicated medical staff of which I am so very proud of at the Be Well Medical Center. We, like so many others, are seeing health care professionals, including first responders, step up in harm’s way to help others. I find it interesting that this is happening at a time when the public was losing some trust with the health care system. Hopefully that will change. We are extending our decision to not see patients inside the office until from April 6 to April 20, 2020. This does not include our clinical research patients who can come in for their study visits as previously scheduled, unless they are not feeling well. We have been able to evaluate all of our patients in need through telemedicine visits and that will continue. Routine wellness visits have been cancelled for the time being. Hopefully, we will resume some type of regular operations of seeing patients in the office on a limited basis after April 13. We will keep you updated. We are fortunate (or lucky) that I upgraded our in-office influenza testing platform 3 months ago. The new equipment that we already have will be able to do the 15 minutes point of care COVID results. We have ordered the COVID-19 kits and were told we will have them within two weeks. Our supply of N95 masks was running low and we just received a new supply of them. Things are looking up and we appreciate the long-time relationship with our vendors in order to accomplish this. Again, to help us help you, please request any prescription refills through your pharmacist electronically. Use the HEALOW portal when possible to schedule telemedical visits or manage other requests. We have been responding to our patients very quickly and do not expect that to change. I have often been asked the following questions: When can recovering COVID-19 patients leave isolation, and do they need “return-to-work” letters? As of March 16, the Centers for Disease Control and Prevention (CDC) includes two options: one with testing and one without. cdc.gov • For patients with access to testing, the CDC recommends they remain in isolation until they have an improvement of respiratory symptoms (cough and shortness of breath), no fever (without the use of fever-reducing medications), and two negative test results from consecutive nasopharyngeal swabs taken at least 24 hours apart. Patients who tested positive for COVID-19 but never showed symptoms should wait until it’s been seven days since their positive test result. • For patients without access to testing, the CDC recommends they stay in isolation until it’s been at least seven days since their symptoms first appeared and 72 hours since their symptoms resolved. Some patients may request notes for their employer, either confirming they have tested positive for COVID-19 or confirming they have been cleared to return to work. The CDC’s guidance, as of March 21, is that employers should not require such documentation (www.cdc.gov) because health care providers will be extremely busy during this national public health emergency. To Your Good Health…We Remain. |
Dr. Paul BensonMedical Director of Be Well Medical Center Archives
August 2021
Categories |
Hours
Mon-Wed: 7:30 am - 5 pm
Thurs.: 7:30 am - 8 pm Fridays: 8 am - 5 pm Select Saturdays: 8 am - 12 noon |
Telephone
|
Email
|

 RSS Feed
RSS Feed